Approach to Management and Prevention of Infections in the Asplenic Patient
- Paulo Behar
- Jun 8, 2023
- 5 min read
American, English, and Brazilian Guidelines
Text for Health Professionals and Other Readers
Summary
The spleen filters blood and regulates the immune response. Asplenia increases the risk of severe infections and sepsis. Fever in asplenic patients is a medical emergency. Treatment includes immediate medical attention, empirical antibiotics, and targeted antibiotic therapy when the causative organism is known. Prevention involves patient education, vaccination, occasional prophylactic antibiotics, and precautions during travel. Asplenic patients should be vaccinated against specific bacteria and receive an annual flu vaccination. Additionally, recommendations regarding COVID-19 should still be followed. Travelers should take precautions to prevent certain infections. Finally, specific considerations are made for patients receiving care in Brazil.
Overview and Recommendations
Background
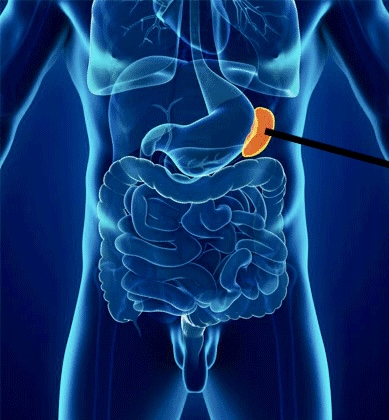
The spleen serves critical functions to filter blood and regulate the immune response.
Asplenia may be congenital (rarely), acquired because of surgical splenectomy, or functional due to a variety of disorders, most commonly sickle cell disease.
Patients with asplenia are at an increased risk for severe infections and sepsis, typically caused by encapsulated organisms such as Streptococcus pneumoniae.
Patients with asplenia may also be predisposed to severe infections with Haemophilus influenzae type b (now rare because of vaccination), Staphylococcus aureus; unusual gram-negative bacteria.
Fever in a patient with asplenia is considered a medical emergency, due to the potential for rapid progression to sepsis.
Management
Advise patients with asplenia and any febrile illness or severe symptoms without fever to seek immediate medical attention.
Empiric antibiotics should target Streptococcus pneumoniae. Ceftriaxone is a reasonable empiric choice for patients who are well-appearing.
Switch to directed antibiotic therapy when the infecting organism and antimicrobial susceptibility is known.
Prevention
Prevention of infections in patients with asplenia involves patient education, vaccinations, prophylactic antibiotics for select patients, and special travel considerations.
Patients should be made aware of the function of the spleen, sepsis and signs of infection, the role of vaccines and antibiotics, and travel-related infections.
Patients with asplenia should be vaccinated against Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis, as well as receive an annual influenza vaccination.
Travelers should notify physicians of travel and take precautions to prevent infections such as malaria and babesiosis.
Prevention of Infections
Education
Asplenic patients and their relatives should be aware that fever represents a medical emergency
counsel asplenic patients to
notify physician and seek immediate medical attention at onset of any febrile illness or severe symptoms without fever
seek immediate evaluation in the event of dog or other animal bite
take appropriate preventative measures when traveling
provide asplenic patients information on
function of the spleen
sepsis, including signs and symptoms of infection
prophylactic vaccines
considerations for traveling
Vaccinations
Recommendations by Infectious Diseases Society of America (IDSA) clinical practice guideline for vaccination of patients with asplenia or sickle cell diseases (2013)
patients with asplenia or sickle cell disease
≥ 2 years old should have
PCV13
PPSV23 ≥ 8 weeks after PCV13 and a second dose of PPSV23 five years later
1 dose of Haemophilus influenzae type b (Hib) vaccine to unvaccinated persons ≥ 5 years old
revaccination with MCV4 (or MPSV4 for those > 55 years old who have not received MCV4) is recommended every 5 years
for PPSV23-naive patients ≥ 2 years old for whom a splenectomy is planned
PPSV23 should be administered ≥ 2 weeks prior to surgery OR
≥ 2 weeks following surgery
immunocompetent household contacts of patients with asplenia (or other immunocompromise)
can safely receive all inactivated vaccines
can get the following live vaccines
measles, mumps, rubella (MMR)
rotavirus vaccine
varicella vaccine
zoster vaccine
yellow fever vaccine
oral typhoid vaccine
should not receive oral polio vaccine
Reference - Clin Infect Dis 2014 Feb;58(3):309
Recommendations by British Committee for Standards in Haematology (BCSH) 2011 guideline for patients with absent or dysfunctional spleen
All patients with functional hyposplenism or history of splenectomy should receive
pneumococcal vaccine
Haemophilus influenza type B vaccine (if not previously immunized)
meningococcal conjugate vaccine (if not previously immunized)
influenza vaccine yearly
Factors associated with high risk of invasive pneumococcal disease in patients with hyposplenism include
age ≤ 16 years old or > 50 years old
inadequate serological response to pneumococcal vaccine
history of invasive pneumococcal disease
splenectomy for hematological malignancy, particularly in context of immunosuppression
patients developing signs or symptoms of infection despite prophylaxis should be promptly admitted to hospital and given systemic antibiotics
consider meningococcal A and C polyvalent vaccine for short-term protection in patients at risk (such as traveling overseas)
vaccine administration
all vaccines should be given ≥ 2 weeks pre splenectomy if possible or 2 weeks post splenectomy
vaccines should ordinarily be given as soon as practicable after recognition of nonsurgical hyposplenism but specific scheduling may be required in the context of recovery from immunosuppression
Reference - British Committee for Standards in Haematology guideline on prevention and treatment of infection in patients with absent or dysfunctional spleen (Br J Haematol 2011 Nov;155(3):308).
Recommendations by Brazilian Ministry of Health
Vaccines for people with clinical conditions that have increased susceptibility to infections of various types (Manual of Reference Centers for Special Immunobiologicals - CRIE)
People with other associated risk conditions that require special immunobiologicals: anatomical or functional asplenia, hemoglobinopathies, storage diseases, and other conditions associated with splenic dysfunction
Severe infections by encapsulated germs, mainly Haemophilus influenzae type b, pneumococcus, and meningococcus, are frequent in these patients.
Although there is no problem with controlling viral infections for these individuals, chickenpox can represent an important factor for secondary bacterial invasion, with a significant increase in morbidity and mortality.
In patients who will undergo elective splenectomy, vaccination should precede the surgical procedure by a minimum period of 14 days. Patients who have already undergone splenectomy show a better response to vaccination starting 14 days after the surgery, but the opportunity to vaccinate should be considered a priority in deciding when to vaccinate. In addition to routine vaccines, these patients need chickenpox, hepatitis A, inactivated influenza, and encapsulated germ vaccines: pneumococcus, meningococcus, and Haemophilus influenzae type b.
In Brazil, the National Immunization Program (PNI) is recognized for its excellence by the World Health Organization. Therefore, a good strategy is to review the patient's vaccination card and recommend that they visit one of the Special Immunobiological Reference Centers (CRIE) to review their vaccination history once more and to administer vaccines according to the PNI. In Porto Alegre, RS, Brazil, there are two locations:
CRIE Maternal and Child Hospital Presidente Vargas Address: Av. Independência 661, Bairro Independência, Porto Alegre/RS. Open Monday to Friday, from 8 am to 12 pm.
CRIE Sanatório Partenon Hospital Address: Av. Bento Gonçalves, n°. 3.722, Bairro Partenon, Porto Alegre/RS. Open Monday to Friday, from 8 am to 12 pm.
The vaccine recently approved by the National Health Surveillance Agency (Anvisa) (2022) for herpes zoster is also recommended. Since it is not yet included in the PNI, refer to a private vaccination clinic for vaccination.
Principais pontos do artigo
Asplenic patients have a higher risk of severe infections and sepsis, usually caused by encapsulated organisms, such as Streptococcus pneumoniae.
The management of infections in asplenic patients includes patient education, vaccination, prophylactic antibiotics for selected patients, and special travel considerations.
The recommended vaccines for asplenic patients include Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis, as well as an annual flu vaccination. And recommendations regarding COVID-19 should still be followed.
In Brazil, refer the patient to a CRIE to update their immunization and for vaccination against Haemophilus influenzae type b, pneumococcus, and meningococcus. Refer the patient to a private vaccination clinic to administer the herpes zoster vaccine.
Blog tips
1. Review the patient's detailed history of previous infectious diseases and vaccination records.
2. Maintain close contact with fellow doctors and other healthcare professionals collaborating on the case, especially the patient's attending physician.
3. Provide a structured written feedback to the colleague who requested the evaluation, if applicable.
4. To do this, briefly check the vaccination schedules in Brazil: all general schedules at https://sbim.org.br/calendarios-de-vacinacao and the specific schedule for special patients at https://sbim.org.br/images/calendarios/calend-sbim-pacientes-especiais.pdf, which is more relevant to this article.
5. Remember which vaccines are provided by SUS, according to PNI, and which are not available in public facilities, so the patient can be directed to vaccination locations.
6. Pay attention to the onset of fever.
7. The vaccination history of family members and other frequent contacts should also be recorded and analyzed.
Paulo Behar
CRM/RS 15273 — RQE 08068
References
Approach to Management and Prevention of Infections in the Asplenic Patient — DynaMed
MINISTÉRIO DA SAÚDE (BRASIL) MANUAL DOS CENTROS DE REFERÊNCIA PARA IMUNOBIOLÓGICOS ESPECIAIS. 5a edição . Brasilia DF 2019. https://bvsms.saude.gov.br/bvs/publicacoes/manual_centros_imunobiologicos_especiais_